Prevent Antibiotic Resistance
Oleh: dr. I Kt. Agus Indra Adhiputra, Sp.MK
Antibiotics are drugs that are not foreign to the public. When receiving a drug prescription, the doctor always reminds you to take antibiotics according to the dose until they run out. Lack of public knowledge about antibiotics results in negligence in their use. The condition that is often found is not taking antibiotics according to the recommended dose. This is very dangerous because it can cause bacteria to become resistant (resistant) to antibiotics, making treatment more difficult.
Antibiotics or what is known as antibacterial is a substance (substance) that has a function to kill or inhibit the growth of bacteria. Historically, antibiotics have been used since ancient Egypt made from plant and fungal extracts to kill bacteria and treat wound infections. At the end of the 19th century, modern antibiotics began to be discovered and developed.
Alexander Fleming, a microbiologist from England accidentally discovered the first antibiotic, namely Penicillin . The discovery of antibiotics occurred when Fleming conducted research on Staphylococcus bacteria . While leaving his laboratory, Fleming accidentally left a petri dish containing Staphylococcus bacteria open. This caused the petri dish to be contaminated by the fungus Penicillium notatum . When he returned to continue his research, Fleming noticed that the growth of bacteria had been hampered by the contamination of the fungus. Research continues to determine the compounds contained in the fungus Penicillium notatumThus was born the first antibiotic called Penicillin . However, subsequent research did not go smoothly. Fleming encountered problems with the cultivation and isolation of these mushrooms, so his research was stopped. Research on Penicillin was then continued by Howard Florey and Ernest Boris Chain. They succeeded in purifying Penicillin so that it can be used to treat various diseases. Because of this discovery, Alexander Fleming was awarded the Nobel Prize in Medicine in 1945 with Florey and Chain.
In 1941, all types of Staphylococcus bacteria were sensitive (sensitive) to Penicillin . However, three years later this type of bacteria is already resistant to Penicillin . Until now, not only Staphylococcus bacteria are known to be resistant to antibiotics, Pseudomonas , Enterococcus , and Mycobacterium tuberculosis bacteria also have penicillin resistance .
Bacterial resistance to antibiotics is the natural ability of bacteria to defend themselves against the effects of antibiotics. Antibiotics become less effective in controlling or stopping the growth of bacteria. Bacteria that are the target of antibiotic surgery adapt naturally to become resistant and continue to grow for survival even in the presence of antibiotics. Bacterial resistance to antibiotics through several mechanisms. Like humans, bacteria have DNA ( Deoxyribo Nucleic Acid ).) so that bacteria can mutate or change. Then, when input from the outside world interacts with the mutation, only the strongest of the variations will survive. When humans use antibiotics to kill bacteria, the bacteria spontaneously mutate their genes which alter their composition in such a way that the antibiotics cannot kill them. These surviving bacteria pass these genes on to bacteria by simple mating (technically known as ‘conjugation’) and bacterial resistance can spread from one living thing to another. Another worrying thing is that bacteria can share these genes with each other by crossing other bacterial species. So they don’t have to be genetically similar to pass on resistance. trillions of different types of bacteria, then pass on resistant bugs to each other which are sometimes referred to as superbugs .
There are two basic things related to the occurrence of bacterial resistance to antibiotics, namely the ability of bacteria to quickly evolve to form self-defense against antibiotics and the contribution of humans in helping these bacteria to evolve more quickly. Human contribution is an important risk factor in bacterial resistance, namely the inappropriate use of antibiotics. Inappropriate use of antibiotics is related to irrational use of antibiotics:
- Frequent use of antibiotics in treatment can reduce the effectiveness of these antibiotics.
- Excessive antibiotics. We can see this in the irrational prescribing of antibiotics to patients even when the patient does not need antibiotics at all, for example when he has a viral infection. Some examples of antibiotics that lose their effectiveness relatively quickly after being marketed due to resistance problems are ciprofloxacin and cotrimoxazole.
- The use of antibiotics in the long term gives an opportunity for the growth of more resistant bacteria ( first step mutant ).
Inappropriate and irrational use of antibiotics is a major problem in bacterial resistance to antibiotics. The cause of this is prescribing the wrong antibiotic with the wrong dose for a particular infection. In addition, there are several medical circles who prescribe broad-spectrum antibiotics to kill bacteria that cause infection so that the target bacteria are more resistant to antibiotics that are not specific for themselves. Another major problem related to the inappropriate use of antibiotics is the availability of antibiotics freely in the market even without a doctor’s prescription. The use of antibiotics that the patient does not understand can also be one of the causes of bacterial resistance. Most patients who receive antibiotic therapy often stop treatment when they feel subjectively better than before or think that they have recovered even though the doctor has given the appropriate dose of antibiotics to take until the bacteria that cause infection can be completely eradicated. This causes the bacteria present in the patient’s body to not be completely eradicated and a new self-defense arises against the same antibiotics that will attack in the future.
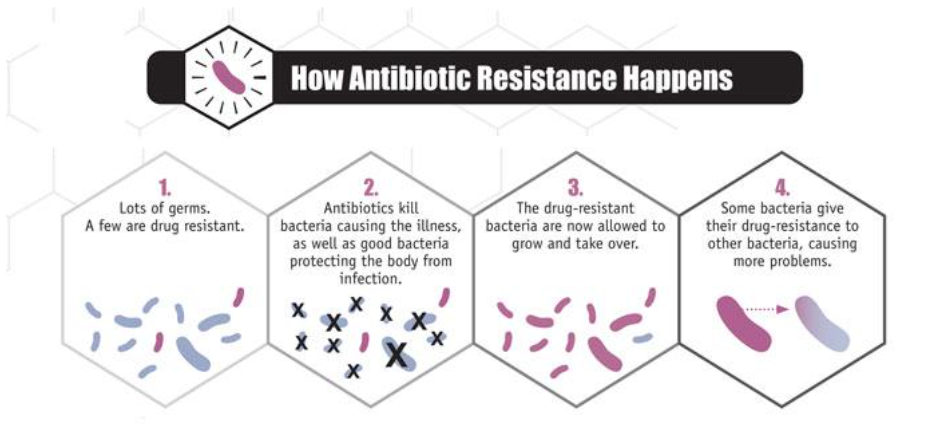
Figure 1. How antibiotic resistance can occur. 1) Many microbes, some of them resistant. 2) Antibiotics kill bacteria that cause disease and also good bacteria that protect the body from infection. 3) Bacteria that are already resistant to antibiotics begin to increase in number. 4) Some bacteria pass their resistance to antibiotics to other bacteria which in turn gives rise to more other antibiotic resistant bacteria. Source: CDC.gov
We can play an active role in inhibiting the occurrence of bacterial resistance, the way is by using antibiotics appropriately. Although antibiotics are very powerful drugs, they are only effective for use against diseases caused by bacteria and not by other microbes. Some useful tips when we go to the doctor, namely first ask whether the antibiotics given are useful for the disease that is being suffered at this time. Second, if you get antibiotics, you must use them until they run out, don’t leave the antibiotics for treatment at a later time. Third, use the antibiotics given according to the doctor’s advice. Use regularly until it runs out even though you feel healthy. If antibiotic treatment is stopped too soon, Then some bacteria can survive and cause infection again. Fourth, do not use antibiotics that are prescribed for others. Sometimes because we feel that the symptoms of the disease are the same, we equate treatment with that person, even though everyone’s needs may be different. Fifth, if the doctor concludes that our illness does not require antibiotic treatment, ask for other treatments that can help relieve the symptoms we feel. Do not force the doctor to give us antibiotics. if the doctor concludes that your disease does not require antibiotic treatment, ask for other treatments that can help relieve your symptoms. Do not force the doctor to give us antibiotics. if the doctor concludes that your disease does not require antibiotic treatment, ask for other treatments that can help relieve your symptoms. Do not force the doctor to give us antibiotics.






